The United States has one of the most expensive health systems in the world, hampering the country’s fiscal and economic well-being. In 2021, U.S. healthcare spending totaled $4.3 trillion, which averages to about $12,900 per person. By comparison, the average cost of healthcare per person in other wealthy countries is less than one-half of that. What’s more, 34 percent of the nation’s healthcare spending is funded by the federal government — placing a strain on the federal budget and contributing to the nation’s growing national debt.
One commonly cited reason for the exorbitant cost of the U.S. health system is waste. Approximately 25 percent of healthcare spending in the United States is considered wasteful, and about one-fourth of that amount could be recovered through interventions that address such waste.
What's Wasteful Healthcare Spending and Where Does It Come From?
Wasteful spending in healthcare is generally defined as:
- Services and processes that are either harmful or do not deliver benefits
- Excess costs that could be avoided by replacing services or products with cheaper alternatives that have identical or better benefits
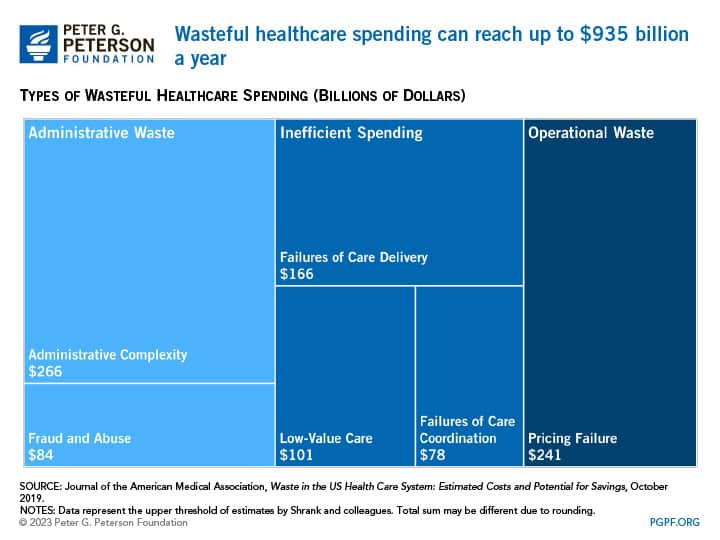
According to a 2019 study by healthcare scholars in the Journal of the American Medical Association, the annual cost of wasteful spending in healthcare has ranged from $760 billion to $935 billion in recent years, or nearly one-quarter of total healthcare spending. Such spending can generally be categorized as administrative waste, inefficient spending on clinical care, or operational waste.
Healthcare Administration Costs Are the Largest Source of Health System Waste
The largest source of health system waste, roughly $266 billion, is due to administrative costs.
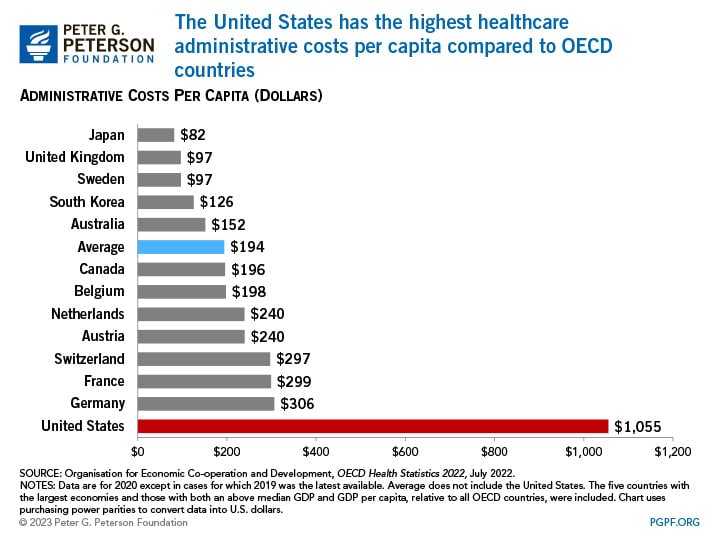
Administrative complexity. The United States spends considerably more on healthcare administration than other wealthy countries. In 2021, the United States spent $1,055 per capita on such costs, while the second highest level of such spending was Germany at $306 per capita. That difference is partially due to the administrative complexity of having multiple payers in the U.S. healthcare system, which results in higher costs associated with billing- and insurance-related expenses, including managing insurance claims, clinical documentation and coding, and prior authorization issues. That administrative complexity is illustrated by the fact that estimated time spent dealing with bill-related matters amounts to $68,000 per physician per year. However, it should be noted that much of the spending discrepancies among countries stem from the fact that the U.S. healthcare system operates differently than other OECD countries, particularly those with single-payer systems.
Operational waste is a smaller portion of wasteful healthcare spending, and it occurs in cases of pricing failure or when medical materials are misused.
Pricing failure. Pricing failure in the healthcare sector translates to inconsistent pricing of care due to different entities paying a range of prices. Prices can depend on facility setting, (e.g., inpatient versus outpatient), location (e.g., rural versus metropolitan), and type of insurance. For example, a 2021 study by the Radiological Society of North America found that the median negotiated price for an MRI scan of the lower spinal canal cost $1,311 when paid in the commercial market compared to $269 for Medicare. Pricing failure often leads to overpricing, and it affects prices for medications, payer-based health services, and laboratory-based and ambulatory services. Because the health sector operates differently than other markets, pricing failure contributes an estimated $231 billion to $241 billion of waste in the healthcare system per year; however, what is considered pricing failure by some studies may actually just be reflecting market conditions in specific areas.
Misuse of medical materials. The misuse of medical materials arises when less expensive but equally effective alternatives are not used or when medical materials are wasted. A common example of using less expensive alternatives is swapping out brand-name drugs for generic ones. When generics or biosimilars become available, they offer less expensive treatment options for patients and payers. In the pharmaceutical sector, waste of medical materials can manifest in large amounts of discarded and unused medicines from redundant prescriptions, patients’ non-adherence to the prescribed course of treatment, and shortcomings of hospitals’ management of drug stock. Researchers estimate that hospitals throw out $3 billion worth of medications annually.
Conclusion
Healthcare costs are a significant driver of the unsustainable fiscal outlook in the United States. The wastefulness or inefficiencies of the country’s healthcare system is a notable factor contributing to costs in that sector. Since the government pays for around two-fifths of all healthcare spending, eliminating wasteful spending, where possible, would aid in reducing the nation’s debt. Fortunately, there are plenty of solutions to explore that would mitigate wasteful health spending and help reduce the financial impact on both individuals and the government.
Image credit: Photo by Getty Images
Further Reading
Quiz: How Much Do You Know About Healthcare in the United States?
The United States has one of the largest and most complex healthcare systems in the world. Take our healthcare quiz to see how much you know about the cost and quality of the U.S. healthcare system.
How Did the One Big Beautiful Bill Act Change Healthcare Policy?
The OBBBA adds significantly to the nation’s debt, but its healthcare provisions lessen that impact by $1.0 trillion.
Infographic: U.S. Healthcare Spending
Improving our healthcare system to deliver better quality care at lower cost is critically important to our nation’s long-term economic and fiscal well-being.


